Medical devices are indispensable tools that help improve the ability to diagnose and treat illnesses, both simple and complex in nature. As technological disruptors become increasingly available in the healthcare industry, medical device manufacturers are developing more advanced devices which necessitates a robust regulatory framework. Among the regulatory agencies, the United States Food and Drug Administration (FDA) has established a stringent regulatory environment to ensure safe, high quality, and effective devices are marketed within the USA. However, navigating these regulations can be relatively daunting, particularly for foreign manufacturers looking to enter the US market for the first time. This blog covers some critical FDA medical device regulations for medical devices in the USA.
US FDA Medical Device Classification
The United States Food and Drug Administration is responsible for regulating the safety and effectiveness of medical devices. FDA’s Center for Devices and Radiological Health (CDRH), established in 1982, is responsible for the oversight of manufacturing, repackaging, relabelling, and/or importing medical devices.
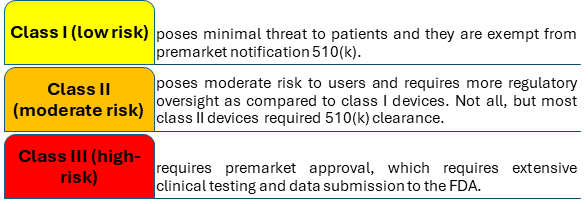
The FDA uses a risk-based classification system to medical device regulations in the USA and divides them into three classes:
What are the Key Regulations Governing Medical Devices in USA?
The FDA has established a comprehensive framework to ensure that medical devices are safe, effective, and manufactured to high-quality standards. This framework includes several key regulations that vary based on the classification of the device.
- Establishment Registration and Medical Device Listing – 21CFR Part 807
The FDA requires all manufacturers and distributors of medical devices to register their establishments with the agency before selling their products. This process is conducted electronically through the FDA Unified Registration and Listing System (FURLS). Further, foreign manufacturers must have a U.S. agent who can act as a point of contact for the FDA. Manufacturers are also required to list their medical devices, providing detailed information about each device, such as manufacturers, contract manufacturers, sterilizers, repackagers, relabelers, specification developers, and others involved in the production or modification of medical devices.
- Premarket Notification 510(k)
Premarket Notification, commonly referred to as 510(k), is a regulatory pathway established by the FDA under 21 CFR Part 807 Subpart E. It allows manufacturers to demonstrate that their medical device is substantially equivalent (SE) to a device that is already legally marketed in the United States.
Manufacturers must submit their 510(k) application at least 90 days before marketing the device. Once submitted, the FDA reviews the 510(k) application to determine whether the new device is SE to the predicate (legally marketed device(s) to which equivalence is drawn). If deemed SE, the FDA issues a clearance letter, allowing the manufacturer to market the device. If not substantially equivalent (NSE), the applicant may resubmit another application/ or De Novo pathway/ or file a reclassification petition / or submit a PMA.
- Premarket Approval
Premarket Approval (PMA) was established by the Food and Drug Administration (FDA) under 21 CFR Part 814. This process is mainly designed for Class III medical devices.
Requirements for PMA:
- Applicants submitting class III medical device applications must provide appropriate scientific evidence to demonstrate the safety and effectiveness of proposed medical devices. This includes:
- Results from non-clinical studies [such as bench testing (which is performance testing like mechanical and biological engineering performance) and animal testing].
- Data from clinical trials that demonstrate the device’s safety and effectiveness.
- Information about manufacturing processes and quality control measures.
- Proposed labeling for both healthcare professionals and patients.
- Investigational Device Exemption (IDE)
The Investigational Device Exemption (IDE) - 21 CFR Part 812 is an exemption that allows manufacturers to gather clinical information on medical devices that have not yet received marketing approval, which can later support applications for premarket approval (PMA) or premarket notification (510(k)).
Clinical evaluation of devices not cleared for marketing requires an investigational plan approved by an IRB or FDA (If the study involves a significant risk device), informed consent from all patients, labelling for investigational use only, monitoring, and required records and reports.
- Quality System Regulation
The Quality System Regulation (QSR), codified in 21 CFR Part 820 ensures that medical devices are designed, manufactured, and distributed in a manner that guarantees their safety and effectiveness.
As of January 31, 2024, the FDA announced the Quality Management System Regulation (QMSR) Final Rule, which amends the existing QSR by incorporating international standards set by ISO 13485:2016. This update aims to harmonize U.S. regulations with global standards for medical device quality management systems. The new rule will take effect on February 2, 2026.
- Labeling requirements
The Labeling Requirements for medical devices are governed by 21 CFR Part 801, which outlines the essential information that must be included on device labels.
The following Parts of Title 21 of the CFR contain labeling requirements for medical devices:
- General Device Labeling - 21 CFR Part 801
- Use of Symbols - 21 CFR Part 801.15
- In Vitro Diagnostic Products - 21 CFR Part 809
- Investigational Device Exemptions - 21 CFR Part 812
- Unique Device Identification - 21CFR Part 830
- Good Manufacturing Practices - 21 CFR Part 820
- General Electronic Products - 21 CFR Part 1010
- Medical Device Reporting
Medical Device Reporting (MDR), governed by 21 CFR Part 803, establishes essential requirements for manufacturers, importers, and user facilities to be promptly informed of significant safety issues related to medical devices.
The Medical Device Reporting (MDR) regulation mandates manufacturers, importers, and device user facilities to report adverse events and product-related problems to the FDA. The regulation requires reports to be filed on Medwatch Form 3500A or an electronic equivalent. The FDA published a final rule in February 2014, requiring e-submission for processing, review, and archiving.
Challenges in the US FDA Medical Device Industry
The U.S. medical device industry is considered as a global leader in innovation, still it faces several challenges, particularly in ensuring the safety and efficacy of devices postmarket. A recent Government Accountability Office (GAO) report, published on August 15, highlights two significant challenges the FDA faces in establishing a robust postmarket surveillance system for medical devices: limited use of unique device identifiers (UDIs) and insufficient funding.
- Limited Use of Unique Device Identifiers (UDIs)
UDIs are crucial for tracking and identifying specific medical devices in real-world settings. While the FDA has mandated their inclusion on product labels since 2013, adoption across healthcare systems remains inconsistent. The limited integration of UDIs in electronic health records (EHRs) and billing systems hampers the ability to efficiently trace devices linked to adverse events or recalls.
This gap complicates safety monitoring and poses risks to patients. For example, UDIs could simplify recall processes, enabling affected individuals to identify problematic devices more easily. Despite advocacy efforts and collaborative initiatives, the FDA lacks the authority to mandate their use in clinical and administrative workflows. The agency has relied on encouraging adoption through coordination with stakeholders and promotional efforts.
- Funding Constraints
The financial burden of establishing and maintaining an active postmarket surveillance system is another pressing issue. The FDA estimates that $8 million is required to operationalize the system, but current appropriations fall short. While the FDA has allocated $5 million from its existing budget, it did not receive the additional $3 million requested from Congress. Without adequate funding, the FDA must divert resources from other critical postmarket activities, potentially compromising broader safety initiatives.
To address this issue, the FDA has proposed alternative funding mechanisms, such as using medical device user fees. However, current laws restrict the application of these fees to postmarket surveillance, necessitating collaboration with Congress and the industry to explore viable solutions.
Conclusion
As the industry continues to evolve with rapid technological advancements, the regulatory landscape must adapt accordingly to address emerging challenges and opportunities. While the complexities of compliance, stringent clinical evaluation requirements, and the need for robust cybersecurity measures present significant hurdles, they also drive innovation and improvement in device quality and safety. These developments promise to enhance the efficiency of the approval process while maintaining rigorous safety standards. Manufacturers must comply with the latest regulatory guidelines and must submit high-quality dossiers to speed up the approval process. As stakeholders work together to address the evolving needs of the industry, the future of medical device regulation holds great potential for enhancing healthcare delivery and patient care.
In addition to providing regulatory services and pharmacovigilance services for global customers, DDReg Pharma offers specialized clinical regulatory services to assist with Clinical Trial Applications in the United States. For further information, connect with our experts. Read more about medical device regulations from the experts here: Regulatory Framework for Software and Artificial Intelligence as Medical Device